Postpartum psychosis

QUICK LINKS:
Symptoms of postpartum psychosis
Management of postpartum psychosis
Recovery from postpartum psychosis
Find local help and support for postpartum psychosis
Download Postpartum Psychosis Fact Sheet
What is postpartum psychosis?
Postpartum psychosis – also referred to as postnatal psychosis or more formally, puerperal psychosis – is a rare condition that affects around 1 to 2 in every one thousand mums. It is a very serious mental health condition that requires urgent attention and treatment.
Postpartum psychosis occurs in the first few days or weeks after a baby is born. While we don’t really know what causes the condition, we do know that women who have a prior diagnosis of bipolar disorder, or who have experienced the condition when having children prior, are at greater risk. Some women may however experience the condition with no prior history.
It is very important that postpartum psychosis is identified and treatment sought urgently as the condition is very serious and places the mother at risk of harming herself, the baby and/or other children – due to its impacts on her thinking and behaviours.
While the onset of postpartum psychosis can be quite daunting, there are good prospects of a full recovery.
Postpartum psychosis is also referred to as postnatal psychosis or more formally, puerperal psychosis. It is a rare condition that affects around 1 or 2 in every thousand mums. It is however, a very serious mental health condition that requires urgent attention and treatment.
Symptoms of postpartum psychosis
Postpartum psychosis (postnatal psychosis) leads to marked changes in the mother’s behaviour, and can be highly distressing both for the mother experiencing them, and their families.
Often, because people are not aware of the disorder or what the symptoms are, when the symptoms occur it can be very confusing and alarming for the mother and family.
Early signs or symptoms of postpartum psychosis
Some of the early signs of postpartum psychosis include:
- Finding it hard to sleep
- Feeling full of energy or restless and irritable
- Feeling invincible – strong, powerful and unbeatable
- Having strange and irrational beliefs such as that someone is trying to harm the baby
These symptoms typically begin to emerge from within 2 days to two weeks after giving birth. In some cases the symptoms can develop later (up to twelve weeks after the baby’s birth).
Over time, this range of symptoms may be followed by a combination of manic, psychotic and/or depressive symptoms which can affect a woman’s energy, thinking, behaviour and mood. If you are noticing these symptoms and they seem out of character for you or your partner, talk to your health professionals about what you have noticed.
Psychotic symptoms
Postpartum psychosis can affect a mother’s thinking and perceptions, resulting in what is known as psychotic symptoms. There are different types of psychotic symptoms. For example, women may state that they are hearing voices or seeing things that are not there (hallucinations) or start to believe things that are not based on reality (delusions).
Manic symptoms
Manic symptoms can include having high levels of energy, racing thoughts and talking quickly. Mania can make it very difficult for a mother to concentrate, and her moods may change in a short space of time.
Depressed symptoms
Depressed symptoms are quite the opposite to mania symptoms. A mother will have little or no energy, and have negative thinking about herself and life in general. Often people with depression describe feeling helpless, hopeless and worthless, and may doubt themselves and their ability as a mother. When depression is severe, it can lead a mother to have thoughts about suicide, or harming herself and/or the baby.
I became euphoric immediately after birth…I had never been SO happy, then I became manic, shopping for baby clothes and decorating the nursery, but by day 13 I had an emotional breakdown and became psychotic and suicidal.
Experiencing or seeing these symptoms can be very distressing – both for the mother herself, and for the partner and other family members. At times like this it is important to remember that these symptoms are all part of the condition which can be treated and managed.
Download Postpartum Psychosis Fact Sheet
Management of postpartum psychosis
Seek help immediately
As postpartum psychosis is a serious mental health condition, it is very important to seek urgent and immediate professional help from a GP, mental health service or hospital emergency department so that timely and appropriate management can stabilise the woman’s energy, thinking, behaviour and moods.
Delays in identification and treatment can mean that treatment becomes longer and more complex. Delays can also pose significant safety risks for both the mother and her baby.
Partners and family members are likely to have to take the lead in accessing treatment. This is because the condition can make it very confusing for the mother and make it difficult for her to see things in perspective; she may not be aware that something is wrong, nor be capable of accessing timely and appropriate help.
In addition to accessing help, partners and family members will also need to continue to play a key role in the mother’s ongoing treatment and recovery.
Find out more about seeking help
Accessing treatment for Postpartum psychosis
Treatment will almost always require admission to a psychiatric hospital. This will allow the woman to be in a safe environment where she can be closely monitored by health professionals.
Some hospitals have mother and baby units which enable the baby to stay with the mother and where both mother and baby can be monitored by health professionals. This allows the mother to remain close to her baby, ensure the needs of the baby are being met and encourages ongoing close contact between them.
Medical treatment
Medication is necessary for the treatment and management of postpartum psychosis to address the chemical imbalance that is leading to the range of extreme symptoms that the woman is likely to be experiencing.
Use of medications requires ongoing monitoring – both on the impact on the mother and her infant. Being in a hospital setting provides this opportunity for close monitoring while the woman stabilises.
A specialist psychiatrist should be consulted when prescribing medications for postpartum psychosis. There are three different types of medications that may be used to treat the range of symptoms.
Mood stabilisers
Mood stabilisers work to stabilise mood and help reduce the likelihood of the symptoms recurring (relapse). The most common mood stabiliser is lithium. Other types of mood stabilisers (which are also used to manage epilepsy) that may be used are sodium valporate, carbamazapine and lamotrigine.
Antidepressants
Antidepressants are used to treat the symptoms of depression that are part of the ‘depression’ part of the disorder.
Antipsychotics
Antipsychotics assist with both manic and psychotic symptoms such as delusions or hallucinations.
It is also important to note that medications should not be prescribed, changed or stopped without discussion with a specialist psychiatrist. They are best placed to assess the risks and benefits of the range of treatments for the mother and her baby.
Medications and Breastfeeding
If breastfeeding, it is important to discuss this with the specialist health professional. Some particular medications (sodium valporate and clozapine) are not recommended. Other medications (such as lithium) should be used cautiously, and their impact on the mother and baby (if breastfeeding) needs to be monitored closely.
I expressed for a while in hospital in the false hope of breastfeeding when I returned home. All milk was tipped down the sink as it was considered unsafe. The reality was that I would be on antipsychotics and mood stabilisers for many months to come and my baby would develop a happy bottle feeding routine with my mother and husband. When I returned home I was able to share in her feeding routine at a pace that suited my very gradual recovery.
As sleep, together with medications, is also an important part of treatment and recovery for postpartum psychosis, the advantages and disadvantages of breastfeeding need to be discussed with your health professional. Doing so can help you make an informed decision about breastfeeding that best meets the needs of the mother, family and infant.
Electroconvulsive therapy
Electroconvulsive Therapy (ECT) is a specialist treatment that may be included in the treatment of postpartum psychosis. By stimulating the neurones in the brain via an electric current, ECT is an effective way of specifically treating the symptoms of mania, psychosis (bizarre thinking) and severe depression.
The only thing that got me out of it was the ECT. I know they had to sedate me to get me to sleep and calm me down but I do feel that they over medicated me and should have just done ECT straight away. I know it’s seen as controversial but I think the stigma around it needs to be removed and people need to understand more about it so they’re not scared of it.
ECT is provided in major hospital settings and the woman is closely monitored to evaluate the impacts of the treatment on the woman’s recovery from postpartum psychosis. Whether the mother and baby are cared for together or separately will depend upon how severe her condition is, the specific needs of the mother and family members and the availability of mother and baby unit beds.
There are safe and effective treatments for postpartum psychosis. Getting help as soon as possible can help reduce the impacts of this serious mental health condition on the mother, her partner, the infant and other members of the family.
Download Postpartum Psychosis Fact Sheet
Recovery from postpartum psychosis
Recovery can be slow, and take time.
Recovering from the most severe symptoms of postpartum psychosis generally can take from between two weeks to twelve weeks (three months) depending on the individual, severity of your symptoms and your response to treatment. The time taken for a full recovery can be much longer and stem from between six to twelve months.
It is recommended that recovery requires a low stimulus environment, with minimum stress and maximum sleep. An extensive network is essential to provide the necessary medical, emotional and practical support. However, too many visitors can be overwhelming.
Recovery and future pregnancies
If you remain on medication over time and are considering becoming pregnant again, it is vital to discuss this with a specialist. If you are taking mood stabilisers, it is also recommended that high levels of folate are taken prior to becoming pregnant and in the first trimester of pregnancy. This can help to reduce the small chance of increased birth defects associated with these medications.
Relapse prevention plan
Developing a relapse prevention plan with a specialist is strongly advised. This can help you and your family identify and prepare, should the condition reoccur.
A relapse prevention plan may also contain information including:
- Your early warning signs – e.g. sleeplessness, elevated mood, very active/busy, skipping meals, being overly suspicious, feeling agitated
- Your vulnerable periods – such as returning to work
- Your self-care strategies – good sleep, daily exercise, eating well, working part time, socialising with friends, taking holiday
- Identifying your sources of help and assistance in advance – this is likely to include additional social supports as well as appointments with specialists throughout pregnancy to monitor your mood and identify and possible symptoms
A tailored relapse prevention and early response plan shared with the treatment team can provide assurance and an important safety net – for the whole family.
I developed an “Advanced Agreement” which provides a basis for responding early to potential relapse. It details my treatment preferences and is shared with my medical team.
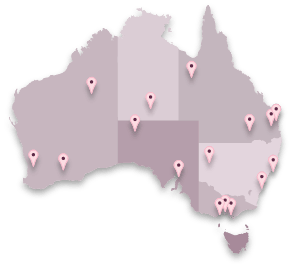
Find local help and support for postpartum psychosis