Managing schizophrenia in pregnancy

Support for schizophrenia during pregnancy
Attending antenatal care is important if you have schizophrenia because relapse is common during pregnancy, especially if you have stopped taking medications. Your doctor or midwife can also give you information about nutrition and ceasing smoking, illicit substance use and alcohol intake in pregnancy.
Treatment for schizophrenia during pregnancy
Talking therapies
Talking therapies can be very helpful in treating symptoms of depression and anxiety. They can help you recognise and change the negative thinking and feelings that depression brings. They also give you useful tools to stop anxiety coming back.
Talking therapies include:
- Cognitive Behavioural Therapy (CBT): the cognitive (or thinking) part of this therapy teaches you to think logically and challenge negative thoughts. The behaviour part helps you change the way you react in situations and can help you to get involved in activities that you have been avoiding or have stopped doing
- Interpersonal psychotherapy (IPT): helps you to find new ways to connect with others, overcome losses, challenges and conflicts that you may have.
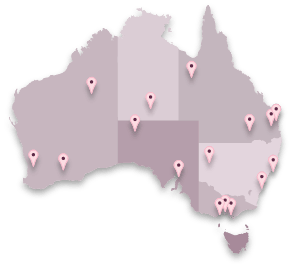
Registered practitioners with appropriate training and experience provide talking therapies for individuals or groups. You can find these types of professionals on the e-COPE Directory.
Medication for schizophrenia
The main medication used to treat schizophrenia are called antipsychotics. These assist with symptoms such as delusions or hallucinations. Some antipsychotics also help improve problems of mood, thinking and socialising and anxiety or agitation. Other than clozapine, antipsychotics can be safely used during pregnancy. As some antipsychotics increase weight gain, it is good to talk to your doctor or midwife about managing your weight.
Depending on your symptoms, your doctor may also prescribe other medicines.
- Antidepressants are used to treat symptoms of depression and/or anxiety. Antidepressants that can be safely used in pregnancy are called selective serotonin reuptake inhibitors (SSRIs). Your doctor may also suggest another type of antidepressant called tricyclic antidepressants, especially if they have worked for you in the past.
- Mood stabilisers help to reduce the likelihood of your symptoms recurring (relapse). The most common mood stabiliser is lithium. Other mood stabilisers that may be used are carbamazepine and lamotrigine. Sodium valproate is not safe for use in pregnancy.
It is important not to change or stop taking your medication without talking to your doctor.
Advice for women experiencing schizophrenia in pregnancy
Seek help and treatment:
- Seek help from a doctor or other health professional.
- Learn about effective treatments.
- Call a support service or mental health crisis line if other help is not available.
Find out about accessing treatment here.
Accept help and support:
- Develop a support system of friends, family and professionals and accept help.
- Discuss your feeling with your partner, family and friends.
Look after your physical health:
- Try to eat healthy meals, including fruit, vegetables, whole grains and lots of water.
- Plan some enjoyable physical activity every day.
- Try to establish good sleeping patterns.
- Practice techniques to reduce stress, such as muscle relaxation and deep breathing.
Advice for family and friends providing support to someone with schizophrenia
Listen and reassure:
- Encourage the woman to discuss her symptoms.
- Explain that schizophrenia can be treated and managed.
Provide information:
- Tell women about the Ready to COPE Guide. This can give them information and support strategies throughout pregnancy.
- Give the woman good quality, evidence-based information about schizophrenia in pregnancy, such as this downloadable fact sheet.
- Give details of helplines if she is feeling distressed and needs support.
- Offer information to the woman’s partner/others.
Direct to care and support:
- Encourage the woman to talk to her general practitioner or other health professionals.
- Encourage the woman to identify and draw on possible supports and services that may be available to her for practical and/or emotional support.
- Remind the woman that she can go to her doctor or local hospital if she is at risk of harming herself or others.
Find out about accessing treatment here.