Postnatal depression

QUICK LINKS:
What is postnatal depression?
Symptoms of postnatal depression
Identifying and diagnosing postnatal depression
Treatment for postnatal depression
Find local help and support for postnatal depression
Download Postnatal Depression Fact Sheet
What is postnatal depression?
Postnatal depression is a common but debilitating condition affecting 1 in 7 women following the birth of their baby.
Having a baby increases the likelihood of developing depression at this time more than at any other time of her life. Unlike the baby blues, which pass on their own, postnatal depression can be long-lasting and affect your ability to cope with a new baby.
Men are also at risk of experiencing distress following the birth of a baby. This is particularly the case if their partner is experiencing postnatal depression.
What does depression feels like?
Depression makes coping and managing from day to day difficult, at any time of life. The additional demands of caring for a baby and/or others can make the impacts of postnatal depression greater. These other demands can also make it hard to find the energy and strength to get on top of postnatal depression on your own.
It was the worst experience of my life. Worse than grief, worse than loss. There was nothing I could do about it, and I was scared it would last the rest of my life.
Symptoms of postnatal depression can develop gradually or within a short period of time.
In some women, depression may develop during pregnancy (antenatal depression) and continue through to the postnatal period (postnatal depression).
For others, postnatal depression will develop for the first time in the weeks or months after the baby is born.
Symptoms of postnatal depression
Understanding the signs and symptoms of postnatal depression can help you to seek effective treatment early
- Feeling low or numb. Some people describe feeling nothing at all
- Lack of interest and/or pleasure in life, yourself and/or the baby
- No energy, finding it difficult to cope and get through the day (may also be attributed to lack of sleep)
- Loss of confidence, feeling helpless, hopeless and worthless
- Often feeling close to tears, highly sensitive to others’ comments or emotional
- Feeling angry, irritable or resentful towards other mothers, the baby or your partner
- Changes in sleep – not being able to sleep even when you have the opportunity, or wanting to sleep all the time
- Changes in appetite, accompanied by weight loss or weight gain
- Difficulties concentrating, thinking clearly or making decisions (which could also result from lack of sleep)
- Feeling isolated, alone and disconnected from others
- Having thoughts of harming yourself, baby and/or other children.
If you are experiencing a number of these symptoms, and these are lasting for two weeks or more in the first year of having your baby, you may be experiencing postnatal depression.
I had a good baby so I thought I shouldn’t really have postnatal depression, but the symptoms were overwhelming, I can recall feeling ashamed of my inability to shower myself and bath the baby every day, and this prevented me from being social, I never asked anyone to visit. We lived in another state from our families, so I knew they wouldn’t be visiting, so I was safe.
Help and treatment for postnatal depression
Postnatal depression is common but it can be serious.
If not recognised or effectively treated, it can become more severe and affect your ability to care for yourself and your baby. And – while it technically develops from the first month up to 12 months after birth – postnatal depression can continue for months or years, or re-emerge in a later pregnancy or following the birth of another child.
Seek professional help immediately if you reach a point where you feel that your partner or baby would be better off without you, or you are having thoughts of suicide or harming yourself or your baby.
Postnatal depression can also have widespread impacts on other family members, including the father or parent, the baby (and their development), and other children.
For all these reasons, it is important to seek help early to reduce these negative impacts.
Postnatal depression can be treated and managed. The faster you seek effective help, the sooner you can recover
How is postnatal depression identified and diagnosed?
Your doctor or maternal and child health nurse may offer your screening with the Edinburgh Postnatal Depression Scale and/or Antenatal Risk Questionnaire.
Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale is a series of 10 questions about how you have been feeling in the last seven days. For each question, you choose the response that describes your feelings.
Antenatal Risk Questionnaire (ANRQ)
The Antenatal Risk Questionnaire asks questions about your life more generally and helps to identify factors that may place you at greater risk of experiencing depression.
If you think you might be experiencing depression, you can ask your doctor or maternal and child health nurse for these screening assessments. Your score(s) will tell you and your doctor or maternal and child health nurse whether it would be helpful to further assess your mental health.
A GP or trained mental health professional can diagnose depression. They do this by asking whether you have had certain symptoms over a period of time (usually 2 weeks or more).
Download our Postnatal Depression Fact Sheet
Treatment for postnatal depression

Practical and emotional support can be very helpful, but often this is not enough to help you to recover. Accessing effective treatment for postnatal depression early is an important step towards recovery.
The type of treatment and time required will vary depending on your personal situation, the severity of your symptoms, and how you respond to treatment. Be mindful that treatment can take time, energy and patience.
The best thing anyone said to me was, ‘This will end, and you will get through it. But there is no quick fix’.
Treatment for mild to moderate postnatal depression
Support Counselling
The opportunity to talk through how you are feeling and thinking with someone who can understand and listen without judgement can be helpful for mild depression. It can allow you to share experiences, help you feel understood and not alone, and develop effective ways to deal with challenges.
I used the group (support) to cry and talk about my feelings of anger, sadness and anxiety. It was the only place I could talk about these things because I was afraid to tell anyone else that I was depressed. I thought they would think I was weird or, worse, that I didn’t love my child.
Psychological treatments
Psychological treatments, sometimes referred to as ‘talking therapies’, can be very effective for the treatment of mild to moderate postnatal depression. These treatments use various techniques to help you identify and manage negative thoughts, feelings and behaviours that are part of postnatal depression, so you can begin to bring your symptoms under control.
Cognitive behaviour therapy (CBT)
Cognitive behaviour therapy can help identify negative thoughts and ways of thinking that commonly occur when someone is experiencing postnatal depression.
If you are depressed, you may view everyday events and opportunities in a negative way – as this is likely to reflect the way that you are feeling. Over time this negative thinking becomes automatic and can maintain not only your negative (depressed feelings) towards yourself, others and/or life in general, but it can also affect your behaviour. For example, you may have negative thoughts about how you look after having your baby, the value of your life, and/or your ability as a new parent. In turn this will affect your feelings towards yourself, others, your interest to engage with others for fear that they too will have a negative view of you. This then may stop you from interacting with others and becoming more isolated. This negative cycle of thinking, feeling and behaviour is likely to make you feel worse over time.
The role of CBT is to teach you how to identify, rationalise and manage your negative thinking and challenge these thoughts and beliefs you may hold. This then gives you greater opportunity to become more objective and positive in your thinking, which will have a positive flow on effect for the way you feel and what you do.
Cognitive behaviour therapy also typically involves setting some goals and activities to also provide you with an opportunity for some positive influences and experiences in your life.
Interpersonal therapy (IPT)
As postnatal depression can be associated with previous losses and/or may be affecting your relationships with others, interpersonal therapy can provide helpful strategies to help you resolve these issues which, if present, are likely to be affecting your postnatal depression.
These two types of therapy can be provided either in groups or individually.
Treatment for moderate to severe postnatal depression
Medical treatments
Antidepressant medication
If your symptoms are moderate to severe, then you may require medication to help provide relief from some of the symptoms of postnatal depression.
When I understood about medication, and got all the information, I was willing to accept it… Before that I was scared of the thought of taking depression medication.
Antidepressants are an effective treatment for postnatal depression. Research and guidelines recommend that there are certain types of antidepressants known as selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs) that can be safely used when breastfeeding, as these medications pass into breast milk at very low levels.
If you are prescribed antidepressant medication, it is important that you take your medication regularly, and as prescribed for it to work effectively. It is likely that it will take up to three to four weeks to feel a positive effect on your mood, and up to six weeks for the antidepressants to have their full effect.
When I took the medication, after a while my mood lifted. I wish that I had known that it took time – it would have made the waiting easier. I was afraid that they were not going to work for me.
While you may experience some mild side-effects during this time, medications can certainly provide relief from symptoms of postnatal depression. And because people respond in different ways, you may need to try more than one type of antidepressant to find the most effective treatment that causes the least side-effects.
The length of time you may need to take medication also varies from person to person. This is likely to be affected by your personal history, the severity of your postnatal depression, other stressors and available supports.
Once you feel that you are at a point of recovery, it is important that you don’t stop taking your medication suddenly. Instead, discuss this with your doctor and work out a plan. Usually antidepressant treatment should continue for between six months to two years after a full recovery is achieved. It can also be valuable to be aware of your initial symptoms of depression to help you identify any signs of possible relapse when coming off medication, or further down the track. This way, you respond early and potentially prevent the condition becoming severe again.
Electroconvulsive Therapy (ECT)
Electroconvulsive therapy or ECT, is a specialist treatment that involves activating electro-currents to the brain. It can relieve a range of severe symptoms of postnatal depression and is generally prescribed if your postnatal depression is severe and medications are not having a positive effect.
My postnatal depression spiralled downwards extremely quickly. I became suicidal and had ECT because the medications weren’t working fast enough.
The number of ECT treatments will vary depending on the severity of your postnatal depression and how rapidly you respond to the treatment.
While ECT may be considered a last resort for many parents, it can certainly be a life-saver as it can effectively provide relief from the symptoms of postnatal depression. There can be side-effects such as short-term memory loss, however this is weighed up by you and your health professional when considering the benefits of ECT for you.
I suffered memory loss from this treatment, and about six months are just gone, including the three months I spent in hospital in the Mother/Baby unit. It’s quite possible that I received more help and information than I can recall. In the end though, it is what got me through.
Download our Postnatal Depression Fact Sheet
Nia’s experience of postnatal depression
In this episode of YouTube and podcast series The Mum Drum, Nia gives a raw and candid account of living with postnatal depression, and what encouraged her to finally seek help:
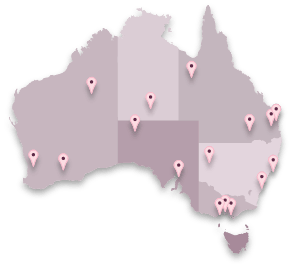
Find local help and support for postnatal depression